Abstract
Introduction: The incidence of feto-maternal complications during pregnancy is high in women with sickle cell disease (SCD) which is the most common inherited hematologic disorder worldwide. Evidence on the impact of transfusions in pregnancy with SCD is lacking with only 12 observational studies and 1 RCT to date that has led to conditional recommendations for transfusional support in pregnant SCD patients. We aim to retrospectively chart review pregnant patients with severe sickle cell disease (HbSS and HbSβ0-thalassemia) and assess if scheduled red cell partial exchanges (RCE) impacted lab values, number of hospital and ED visits, prenatal, perinatal and postnatal outcomes.
Methods: We identified 42 adult pregnancies (40 HbSS and 2 HbSβ0-thalassemia) between 04/2012 and 04/2022. HbSC and HbSβ+-thalassemia patients were excluded from the study as most patients did not get RCE due to overall less disease severity. Patients who received RCE had one unit of phlebotomy followed by one unit of packed red cell transfusion every 2 weeks as per the protocol followed at our institution. Collected data included demographics, lab values, number of hospital admissions/ED visits, prenatal, perinatal, and postnatal outcomes. Descriptive statistics as means and percentages, individual samples t-tests for comparison of means, chi-square tests for associations were utilized to report the data. A p value of <0.05 was considered significant. A binary regression model was utilized to adjust for demographics and comorbidities.
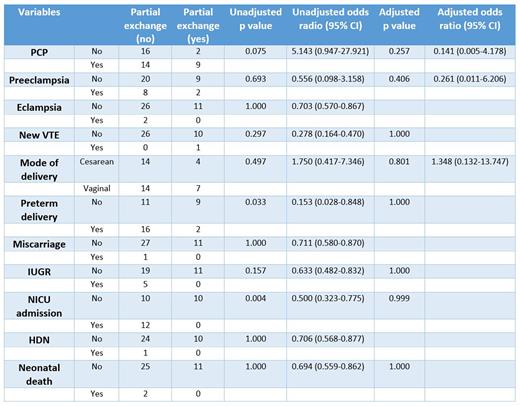
Results: Mean age in the study group was 24.86±4.28 years. All 42 patients had medicare or medicaid. 11/42 (26.2%) patients received scheduled RCE with 73% compliance rate and no documented evidence of allo-immunization. Only 1/37 (2.7%) patients had venous thromboembolism. Patients who received scheduled RCE had higher hemoglobin (Hb) nadirs (7.80 g/dL vs 6.78 g/dL; p .02), lower number of hospital admissions for painful crises (1.00 vs 3.54; p .02) and higher gestational age in weeks at delivery (37.09 vs 33.64; p .007). The differences in means of other hematological and chemistry lab values were insignificant. Scheduled RCE was associated with lower incidence of preterm deliveries and subsequent NICU admission with unadjusted odds ratios of 0.153 (0.028-0.848) and 0.500 (0.323-0.775) respectively. There was no statistically significant association with respect to other prenatal, perinatal or postnatal outcomes such as preeclampsia, eclampsia, mode of delivery, intrauterine growth restriction or neonatal death. Binary logistic regression did not show any statistically significant associations when adjusted for demographics and comorbidities (Table 1).
Conclusions: Pregnant patients with SCD who have had previous pregnancy complications, high hospital admission rates or low Hb nadirs might benefit from scheduled RCE or simple transfusions. Given limited sample size in all 12 reported observational studies, there is a need for multicenter study especially from centers in areas with higher prevalence of SCD. While the TAPS-2 trial was registered in 2019 in the UK and is currently recruiting patients, more trials are necessary to solidify evidence.
Disclosures
Master:Cardinal Health: Membership on an entity's Board of Directors or advisory committees; Aptitude health: Membership on an entity's Board of Directors or advisory committees; curio sciences: Membership on an entity's Board of Directors or advisory committees; Blue Bird Bio: Current holder of stock options in a privately-held company; Toxicity: Current holder of stock options in a privately-held company; Gilead: Current holder of stock options in a privately-held company; Jasper: Current holder of stock options in a privately-held company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal